Causes Of Pelvic Pain And Treatments
Do you experience a sharp, shooting pain in your pelvis that comes on suddenly? Do you have a twisted or knotted feeling when exercising or having sex?
If so, you may be experiencing pelvic pain.
What Is Pelvic Pain?
Pelvic pain manifests in the lower part of your abdomen. It may be constant, come on suddenly, or be acute. You may feel a dull or severe, sharp, stabbing pain that cripples you. If it lasts longer than six months, showing no signs of improvement, you may be dealing with “Chronic Pelvic Pain” (CPP).
Pelvic pain affects 1 in 7 women, and it may indicate an issue with the reproductive system, such as the ovaries or fallopian tubes. However, it occurs in both sexes and can indicate a prostate problem in men.
This type of pain goes beyond the physical; it can also be psychologically motivated, brought on by high levels of depression, anxiety, neuroticism, and sexual abuse.
Causes Of Pelvic Pain
Pelvic pain causes may include:
- Appendicitis: It puts pressure on the pelvis, causing non-gynecological pelvic pain.
- Benign Prostatic Hyperplasia (BPH): Brought on due to an enlarged prostate (not related to cancer), it can cause pain in the pelvis.
- Bladder disorders, such as Urinary Tract Infections (UTIs) or interstitial cystitis, can cause pain and swelling in the lower abdomen.
- Hernia: It can cause sharp, shooting pain at the location specific to the defect, which could be at the pelvic floor. It can get worse when a person coughs, laughs, or does anything that might press against the muscles.
- Intestinal disorders, such as diverticulitis, can cause severe abdominal or pelvic pain.
- Kidney infection or kidney stones can cause unbearable pain in the groin, pelvis, and lower abdomen.
- Nerve conditions, such as Pudendal Neuralgia, can cause pain, discomfort, at times, even numbness in your pelvis.
- Pelvic fracture or disorder.
- Prostatitis: Inflammation or infections in a man’s prostate can often cause pelvic or perineal pain.
- Sexually transmitted diseases: They can cause complications like pelvic pain and pelvic inflammatory disease.
In women or those Assigned Female At Birth (AFAB), it may also arise due to:
- Cancers of the reproductive tracts
- Certain types of cancers, such as cervical, ovarian, or uterine cancer
- Endometriosis
- Menstrual cramps
- Miscarriage or threatened miscarriage
- Twisted or ruptured ovarian cysts
- Ovulation
- Pelvic Inflammatory Disease (PID)
- Pregnancy (ectopic or otherwise)
- Ruptured fallopian tube
- Uterine fibroids
Symptoms That Are Suggestive Of Pelvic Pain
Some of the most common symptoms of pelvic pain include:
- Bloating or gas
- Constipation or diarrhea
- Menstrual pain
- Dysuria—discomfort when urinating
- Pain during sex
- Pain in the hip or groin area
- Vaginal bleeding, spotting, or discharge
- Worsening of menstrual cramps
If the physical condition is severe, you may also:
- Find blood with a bowel movement or in urine
- Develop a fever or chills
- Be unable to stand up straight due to the pain
How Is Pelvic Pain Diagnosed?
The diagnosis of pelvic pain starts with a consultation, where the healthcare provider reviews your medical history and asks questions about the pain, such as:
- Where do you feel the pain?
- When did you first start experiencing the pain?
- How long does the pain and discomfort last?
- Where is your pain located?
- Does your menstrual cycle affect the intensity of your pain?
- Does the pain occur during sexual activity?
- Do you experience anxiety or feel stressed or depressed?
- Have you been touched against your will?
The information you provide will help the doctor make an accurate diagnosis. To support their findings, your provider may use the following diagnostic tools:
- Blood or urine tests to check for blood count, pregnancy (in women of reproductive age), or urinary tract infection.
- Bone density screening for the diagnosis of osteoporosis, as it may be the cause behind the pain in the pelvis.
- Colonoscopy to view the lining of the colon, detect polyps, and remove them to tackle pelvic pain and early cancers.
- CT scan or X-rays of the abdomen and pelvis to detect and diagnose the cause of pelvic pain.
- Diagnostic laparoscopy, if your healthcare provider thinks lesions or adhesions are the cause of your pain. They may also use MRI as an alternative to identify obscured regions in the presence of bowel gas.
- Stool test to check for microscopic blood.
- Vaginal or penile cultures to test for sexually transmitted infections like gonorrhea and chlamydia.
- Ultrasound to create pictures of your uterus, allowing diagnosticians to check its structure and check for abnormalities that may cause pelvic pain.
Hysteroscopy, a minimally invasive procedure, may also be used. It allows the doctor to look at the inside of the uterus to check for gynecological causes of chronic pelvic pain.
Treatments For Pelvic Pain
Treatment for pelvic pain will depend on the cause and extent of your condition, your medical history, and your expectations of the treatment.
Common treatments may include:
- Acupuncture: When combined with pelvic floor rehabilitation therapy, this alternative medicine could help relieve pain.
- Lifestyle changes: Maintaining good posture, quitting smoking, which may be associated with reduced blood flow to pelvic muscles, and nutrition therapy (supplementing vitamin or mineral deficiencies) may help soothe your discomfort and relieve pelvic pain.
- Medicine: Doctors may prescribe over-the-counter pain relievers like aspirin or Tylenol and certain antidepressants like amitriptyline, a tricyclic antidepressant, to treat lower abdominal pain. Antibiotics and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) like ibuprofen, can also ease painful symptoms.
- Physical therapy: Stretching, massages, and exercises can help achieve ease and tolerance in movement to treat chronic pelvic pain (CPP) by enhancing flexibility and mobility. It could be administered with transcutaneous electrical nerve stimulation (TENS) to treat pain.
- Relaxation exercises: Yoga poses may address a hypertonic and hypotonic pelvic floor to alleviate pelvic pain. Mindfulness meditation may also improve outcomes. They also calm emotions, which can improve your quality of life.
- Surgery: If your chronic pelvic pain stems from an issue with your pelvic organ(s), your doctor may recommend laparoscopic surgery to remove the adhesions or tissues causing pain. However, if the problem is severe, you may have to get your uterus, ovaries, or fallopian tube removed via hysterectomy.
Pain and suffering from pelvic pain can drastically lower your quality of life, affecting sleep, decreasing productivity, and increasing stress levels. It’s why 35-45% of people living with chronic pain experience depression and mood fluctuations.
If your doctor feels that your physical pain is intertwined with your mental health or brought on by sexual abuse, they may refer you to a trained psychiatrist.
The Takeaway
Pelvic pain can impair your quality of life and wreak havoc on your mental health.
So, if you notice pain in your lower abdomen worsening over time, make an appointment with a doctor at your earliest convenience. Depending on the cause of your pain, the doctor will prescribe an appropriate course of treatment to help get your life back on track.
The power of protein on weight management
Weight management can be a challenging journey for many individuals, but with the right approach, achieving a healthy and sustainable weight is possible. Among the various factors that influence weight loss success, the role of protein cannot be overstated. Protein is...
Endometriosis: What It Is, Symptoms, Risk Factors, and Treatment
Endometriosis affects more than 11% of American women between the ages of 15 and 44 years as well as roughly 10% of women globally according to the Women’s Health division of the U.S. Department of Health and Human Sciences. Notoriously common and painful, this health...
Unveiling the Health Secrets Within: Understanding the Gut Microbiome
The human body is home to trillions of microorganisms, forming a complex ecosystem within our gastrointestinal tract (GIT) known as the gut microbiome. Long overshadowed by the spotlight on human cells, this intricate community of bacteria, viruses, fungi, and other...
Exploring the Connection Between Cortisol, Stress, and Overall Health
The “Longevity” game is not about living long, but living “well”. And the hidden player calling the shots might be cortisol, aka the stress hormone. As stress permeates our lives, its effects on our overall health become increasingly apparent. In this article we will...
Managing Stress with Diabetes Made Easy: Tips That Tip the Scale in Your Favor
Over 537 million people around the world live with diabetes. The condition affects a whopping 10.5% of the adult population, and there’s no denying how difficult it can be to manage it. One day, you’re living life to the fullest—eating your favorite cake, regularly...
Exploring the Interplay Between Cancer Risk, Physical Activity, and Obesity: Unveiling the Pathways to Prevention
In an era where health consciousness is gaining paramount importance, the relationship between cancer risk, physical activity, and obesity has emerged as a significant area of investigation. As you and I - and many of our friends - are impacted by this scary disease,...
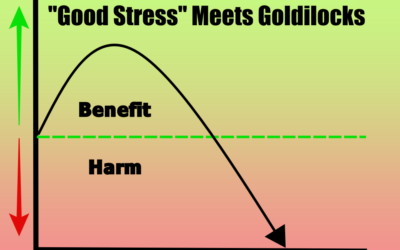
Hormetic Stress: The Good Stress For A Happy Healthy Life
It’s so easy to be tempted by the allure of comfort. In fact, technology and society have convinced us that this is of the upmost importance. You’re cold? Turn on your thermstat. Don’t like that noise? Drown it out with “white noise”. Feeling hungry? No problem. The...
Sarcopenia: Impact on health and longevity
Implications Of Sarcopenia On Health And Longevity It is easy to assume that losing some strength is a “normal part of aging”. In fact, maybe you have even heard this from your healthcare providers. The truth is that getting “weaker” as we age is not “normal” and...
What Is Urinary Incontinence, What Causes it, And How Do You Treat it?
What Is Urinary Incontinence, What Causes it, And How Do You Treat it? Are you experiencing urine leaks, or do you have the urge to urinate every few minutes? If so, you may be suffering from urinary incontinence, a condition that affects over 13 million Americans. It...
Is Reverse Osmosis Water Filtration Better For You?
Water is essential for life, but not all water is created equal. Tap water can contain harmful contaminants and chemicals that can have adverse effects on our health. This is where reverse osmosis water purification comes in. Reverse osmosis (RO) is a highly effective...