Around 40% of women worldwide experience pelvic organ prolapse. Most of them are between 60 and 75 years old. While it is common in those who are assigned female at birth (AFAB), it can also occur in people with penises.
Though it isn’t infectious, it’s an epidemic in its own right — affecting millions of people every year. Knowing what it is can help you take the right steps at the right time to preserve your quality of life.
First, What Is Pelvic Organ Prolapse?
Pelvic organ prolapse is a form of pelvic floor disorder. With this condition, pelvic floor muscles, ligaments, and tissues can no longer support the organs in the pelvic area. Together, they act like a sling that keeps organs — like your bladder, rectum, small bowel, uterus, cervix, and vagina — in place. If they become weak or damaged, these organs can shift from their normal location and press into the vagina, extending outside the vagina or anus and causing a bulge in severe cases.
Pelvic organ prolapse is not inherently life-threatening. In mild cases, you won’t even be able to tell you have a prolapse. However, it can cause pain and discomfort, affecting your quality of life in more severe cases.
Pelvic Organ Prolapse Symptoms
Symptoms vary based on where the prolapse is located.
Here’s a general list of symptoms of uterine prolapse and other types of prolapses:
- A feeling of heaviness, pressure, and aching in the pelvis
- Backache or pain in the lower back
- Constipation or problems with bowel movements
- Discomfort or numbness during physical activity
- Dyspareunia or painful intercourse
- Stress incontinence, a chronic urge to urinate, and other issues with peeing
- Feeling or seeing a bulge, the sensation that something is falling from your vagina
- Problems inserting tampons
- Vaginal spotting
In most cases, symptoms are mild and almost tolerable in the morning but they can worsen as the day progresses which can severely impact your day-to-day life.
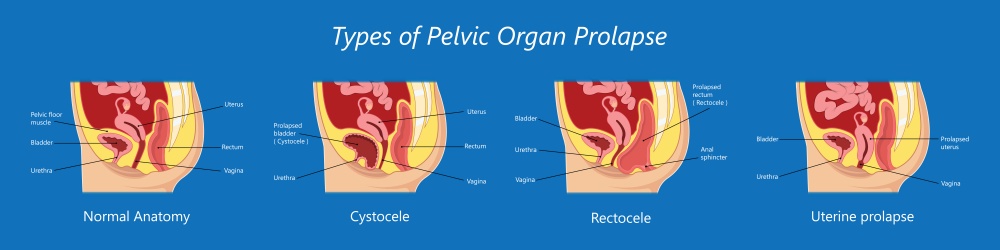
Types of Prolapse
The type of prolapse you have depends on the pelvic organ affected.
The most common types include:
- Cystocele (dropped bladder): The most common type of pelvic organ prolapse wherein the ligaments and muscles supporting the bladder and vaginal wall weaken, causing them to sag or bulge out of the vagina.
- Enterocele (small bowel prolapse): It occurs when part of the small intestine descends into the lower pelvic area, creating a bulge at the top part of the vagina.
- Rectocele (posterior vaginal collapse): This happens when the wall of supportive tissue between the rectum and vaginal wall weakens. It causes the front wall of the rectum to bulge (herniate) into the vagina.
- Uterine prolapse: This condition occurs when the muscles around your uterus become weak. As they can no longer adequately support the organs they hold, they can lead to three types of uterine prolapse based on their intensity, ranging from the uterus slipping down and dropping down into the vagina to pushing the entire uterus out of the vagina.
It’s possible to have more than one type of prolapse at the same time.
Causes of Pelvic Organ Prolapse
Common causes of uterine prolapse and other prolapses in the pelvis include:
- Pregnancy and childbirth which can cause the muscles and tissues supporting your organs to stretch and weaken. Almost 1 in 2 women who have had a pregnancy are at risk for prolapse years after childbirth.
- Giving birth to a large baby (more than 8.5 pounds) or having multiple vaginal deliveries.
- Increased, long-term pressure on your abdomen, which can happen if you’re overweight or obese, suffer from a chronic cough, are experiencing pelvic organ cancers, find yourself straining during bowel movements (constipation), had a hysterectomy, or frequently lift heavy objects.
- Loss of estrogen during and after menopause
- Family history. AFABs with a family history of hernia are 4 times more likely to have pelvic organ prolapse.
Pelvic organ prolapse can also be a normal part of aging in older women.
Conditions brought on by collagen irregularities, such as joint hypermobility syndrome, Marfan syndrome, and Ehlers-Danlos Syndrome, can increase your risk of pelvic organ prolapse.
When To See a Doctor?
If you have any symptoms of pelvic organ prolapse, see a medical practitioner ASAP. Your doctor will ask about your medical history, then conduct an internal pelvic examination with a speculum to check for redness, swelling, lumps, and other irregularities in the cervix, fallopian tubes, ovaries, rectum, uterus, vagina, and vulva. You may also be asked to strain or cough to diagnose the extent of your pelvic organ prolapse.
Additionally, they may conduct other tests like:
- Bladder function tests like cystoscopy and urodynamics, which focus on the bladder’s function and efficiency at holding and emptying urine.
- Imaging procedures like ultrasound and MRI allow your doctors to see the organs inside your pelvis, including the uterus, cervix, fallopian tubes, and ovaries, so that they can confirm problems in your pelvic region.
- Intravenous pyelogram — an x-ray of the urinary tract that evaluates your kidneys, bladder, and ducts (ureters)
- Voiding Cystourethrogram (VCUG) uses a form of real-time X-ray to look at the size and shape of your bladder and how well it functions.
You may also be asked to get a non-invasive pelvic CT scan to help physicians diagnose your medical condition.
Prolapse Treatment Options
Treatment for pelvic organ prolapse includes surgical and nonsurgical procedures. The options available to you will vary based on multiple factors, such as:
- Age
- Overall health
- The type and severity of the prolapse
- Whether you plan to have sex (and children) in the future
Lifestyle Changes
Here are some lifestyle changes that can keep the condition from progressing:
- Lose weight
- Avoid heavy lifting
- Prevent or treat constipation
Pelvic Floor Exercise
Kegel exercises improve the contraction and release of muscles, strengthening your lower pelvis.
Pessary
A pessary is a removable silicone device inserted into the vagina. It can support sagging organs, making it useful for cystocele and rectocele.
Surgical Treatments
If you’re experiencing severe symptoms that are impacting your quality of life, you may need to consider surgery. During surgery, the affected tissue or organ can be repaired, removed, or shut. Treatments can include:
- Colpocleisis: This procedure involves closing the vaginal canal to keep your pelvic organs in place. It’s a good option for women who don’t wish to have vaginal intercourse.
- Colporrhaphy: Depending on where the problem lies, it can treat the interior or posterior vaginal walls by strengthening and tightening the connective tissues that support your bladder and vagina.
- Sacrocolpopexy or Sacrohysteropexy corrects prolapse in the middle of the pelvic floor by creating an incision through the abdominal floor and attaching a synthetic mesh. It is effective in 90 out of 100
Your doctor may also recommend a uterosacral or sacrospinous ligament fixation — a type of transvaginal tissue repair that restores vaginal support.
In Conclusion
Pelvic organ prolapse can negatively affect your quality of life so it’s best to take a proactive approach and try to halt its progression if not curb it altogether. That means maintaining a healthy weight, eating high-fiber foods to avoid constipation, doing Kegel exercises daily, and avoiding heavy lifting and smoking.

