Many have a hard time falling asleep or achieving restful sleep after experiencing a stroke. If you or someone you care about has experienced one, there are ways to get to sleep faster and sleep more soundly.
In this article, we’ll review the types of sleep disorders and issues that can arise after a stroke and enumerate some treatments that may help.
Sleep Disorders and Stroke Survivors
In 2010, the American Heart Association (AHA) developed and publicized risk factors for cardiovascular health and stroke called “Life’s Simple 7.” In their list, they included the consumption of tobacco, diet, blood pressure, physical activity, body weight, cholesterol, and blood sugar levels.
The list, however, failed to include sleep disorders like sleep apnea as well as irregular and excessive sleep patterns as part of routine tests for patients who experienced a stroke. Since many survivors experience problems with sleeping after their strokes, the AHA agrees that sleep should be added as a metric to existing cardiovascular tests. This addition can help identify patients who are at risk for heart problems while helping stroke survivors sleep better after the incident.
We dive into the most common sleep disorders in stroke patients and how they affect survivors.
Insomnia
While some stroke survivors experience excessive sleep after stroke, others have trouble falling asleep or maintaining an uninterrupted sleep cycle. Insomnia after a stroke can be caused by stress, depression, brain damage, or certain heart medications. Stroke survivors who experience disrupted sleep, insomnia, nightmares, waking up too early, or crippling cramps while sleeping should speak to their doctor if clonidine, beta-blockers, or diuretics have been prescribed for hypertension.
It’s important to further investigate this since a continued lack of restful sleep can increase the risk of another stroke. Getting enough sleep after a stroke is essential to support neurogenesis, the formation of new neurons that heals the brain after an episode.
Doctors can suggest alternative medicines as part of post-stroke insomnia treatment. Other options include the following:
- Sleeping in a quiet room with no light (use light-blocking curtains and keep your phone on do-not-disturb mode during sleep)
- Cognitive-behavioral therapy (CBT) may help to lessen the severity of insomnia
- Certain antidepressants such as Zolpidem and Mianserin may encourage better sleep in insomniacs with fewer negative effects on cognitive and motor skills
- Stroke patients should evaluate the risk of consuming hypnotics or psychoactive drugs such as benzodiazepines, which are known to increase the risk of falls and erratic behavior
Excessive Daytime Sleepiness
As important as sleep is for the recovery of stroke patients, many individuals experience excessive daytime sleepiness (EDS). Deep sleep after stroke is normal since the brain is struggling to recover from an episode. However, if you continue to experience EDS months after a stroke, it’s best to speak to your doctor about prescribing stimulant medication to balance EDS.
The following conditions can worsen EDS:
- Reverse Robin Hood Syndrome: This syndrome is a biological process that occurs in the brain when it tries to redirect blood from the affected parts of the brain to non-damaged parts.
- Sleep Apnea: This condition disrupts breathing patterns and can lead to choking, gasping, and loud snoring during sleep. It can also stop a person from breathing for several minutes, obstructing the body’s ability to receive adequate oxygen.
- Depression: For stroke patients, depression can have a debilitating effect on sleep, causing severe drowsiness and fatigue during the day.
Sleep-Wake Cycle Disorder
This disorder affects the 24-hour sleep-wake pattern of a person. For most, the goal is to get at least 8 hours of rest at night and staying awake for 16 hours during the day. The body controls this cycle through its circadian rhythm and its natural ability to maintain sleep homeostasis (when the drive to sleep increases).
Since we’ve developed the habit of remaining awake in the day and asleep at night, it turns into a routine that the body depends on. For stroke patients, the sleep cycle can significantly change. Individuals who have suffered an episode tend to sleep at odd hours and aren’t able to stay awake for long during the day.
How To Improve Sleep After a Stroke
After a stroke, there are ways to improve sleep. These strategies can be practiced simultaneously with a doctor’s prescribed medication and post-stroke therapy. Here are some methods you can try:
- If you suffer from sleep apnea, speak to your doctor about using a C-PAP (continuous positive airway pressure) machine. The machine blows air continuously through a mask, which is worn while you sleep. It is comfortable enough to wear all night and will help your body get adequate oxygen as you rest.
- For those who suffer from sleep-wake cycle syndrome, 30 minutes of bright light therapy daily can help realign your inner clock. Sit in a room with plenty of sunlight, facing the window if you can. Sip on water or tea and allow your body to get accustomed to this daily habit.
- If you have trouble sleeping, talk to your doctor about taking melatonin supplements. Your doctor can recommend whether or not they’re ideal for you based on your medical condition and history as well as the medication you’re taking.
Melatonin is a natural substance that the pineal gland in the brain releases to regulate sleep-wake cycles. Taking it as a supplement can help insomniacs and those who suffer from sleep-wake cycle syndrome.
- Engage in moderate exercise every day to improve cognitive function and mobility.
- If you live in a noisy neighborhood, invest in noise-canceling headphones or a white noise machine for uninterrupted sleep.
- Avoid looking at the TV or your phone an hour before bedtime. Instead, take a warm bath to help relax you.
- Avoid eating a heavy meal right before bedtime to avoid issues such as heartburn, acid reflux, and indigestion. You should ideally consume dinner 3 hours before sleeping.
- During warmer months, your room should be well-ventilated and cool enough to encourage sleep. For colder months, turn on the heater and wear thicker nightwear for better sleep.
- Avoid eating in bed and watching TV. It’s best to have a space dedicated for sleep.
- Drink chamomile or passionflower tea (they contain apigenin, an antioxidant that can help induce sleep) 30 minutes before bedtime.
Conclusion
A stroke can leave you anxious, distraught, and unable to get a good night’s sleep. Sleep patterns can change drastically but there are ways to counteract restless nights with the right medication, therapy, and lifestyle changes.
By first understanding which sleep disorder is prevalent, a doctor can prescribe the best course of action. The above strategies will eventually help improve sleep after a stroke in combination with professional guidance.
Other articles you might like:
Protein: Essential to brain health and repair
Protein, often referred to as the “building blocks of life” is arguably the most critical macronutrient for brain health and repair and disease prevention as we age. One of three macronutrients found in food the body is primarily composed of protein (second only to...
Simple versus Complex Carbohydrates
Carbohydrates are one of the three macronutrients that make up the foundation of our diet, along with protein and fat. They are found in a wide variety of foods, from fruits and vegetables to bread and pasta. Despite their importance in our diet, carbohydrates have...
Brain Health and Recovery: Food IS Medicine
Brain Health and Recovery: Food IS Medicine Food can be an excellent tool to enhance brain health and recovery. However, if you thought the brain was a complicated system to understand, the data on nutrition is far more complicated. So, spoiler, there is no “perfect...
BDNF And Stroke Recovery
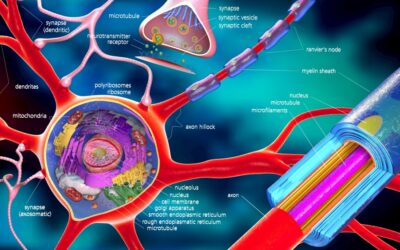
Stroke can cause long lasting disability due to nerve cell (neurons) death greatly impacting someone’s overall quality of life. The neuron death can cause problems with mobility, balance, sensation, speech, vision, cognition (thinking), comprehension (understanding),...
Brain Derived Neurotrophic Factor (BDNF) and Brain Health
Brain-derived neurotrophic factor (BDNF) is a protein that aids in cell function and promotes the growth of new nerve cells (neurogenesis). Studies have shown that BDNF plays a critical role in neuroplasticity (the brains ability to build new nerve connections) and...
Neuroinflammation: Implications in Brain Health and Disease
Neuroinflammation is a broad term that is characterized by an immune response in the central nervous system (CNS) - the brain and spinal cord. This abnormal immune response is initiated by cues including infection, bacteria, brain injury, toxins and autoimmunity. ...
Mitochondrial Dysfunction in Multiple Sclerosis
Multiple sclerosis, also known as encephalomyelitis disseminata is a neurodegenerative disease characterized by damage to the white matter in the brain and spinal cord (central nervous system. The mitochondria are implicated in MS disease progression. With that said,...
Mitochondria: Key to Brain Health
Within every cell of the human body is a pool of structures called mitochondria, often referred to as the “powerhouse” of the cell (generating 90% of the body’s energy). In recent years mitochondria have been credited for brain health and optimal performance. On the...
Exercises to Lift a Stiff/Heavy Leg
https://youtu.be/4Op-qbT4yjo Following a neurologic injury, some people experience a leg that feels stiff, heavy, or both. This can make walking difficult. In this video, you will learn the best exercise routine to relearn how to lift the leg more efficiently and...
Dysphagia after stroke
Dysphagia After A Stroke Over 50% of patients are affected by dysphagia after stroke. It is typically characterized by the inability to swallow liquids or foods and can lead to choking. Patients usually tend to recover from post-stroke dysphagia within the first week...